Asthma: Take Control- Don’t Let Asthma Control You!
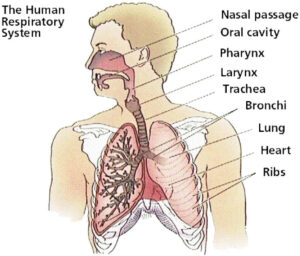
When you breathe, air travels through tubes (bronchi , bronchioles) in your lungs
to reach tiny air sacs (alveoli) so that your body can get the oxygen it needs.
What Causes Asthma?
Asthma is a chronic condition in which the lining of the airways, or bronchial tubes, is inflamed and overly sensitive to many factors which “irritate” them. Exposure to one of these irritating factors can cause symptoms in a person with asthma.
What Are “Asthma Triggers”?
Factors which irritate the airways and cause asthma symptoms arc called “asthma triggers.” Many substances or events can trigger chest tightness, coughing, and wheezing. Some triggers are common for many people including:
- Respiratory infections
- Exercise
- Cold Air
- Cigarette smoke
- Odors, perfumes, aerosols
- Air pollution
- Allergens
- Emotional stress
- Fatigue
- Weather changes
- Gastroesophagcal Reflux Discasc/LPR
What are Early Warning Signs?
Many patients notice a variety of symptoms that occur before the onset of chest symptoms. Examples include:
- Fatigue
- Irritability
- Itching of chin or back
- Dark circles under the eyes
- A drop in your peak flow values
It is important to identify and recognize these early warning signs and to intervene before asthma symptoms progress.
How Do My Asthma Medications Help?
Medications used to treat asthma can be grouped into two broad categories based on how they work to relieve or prevent asthma symptoms.
Quick -Relief (Rescue) Medications: Bronchodilators
Rescue medications open the airways by relaxing the muscles surrounding the bronchial tubes.
- Beta-agonists: inhaled short acting beta-agonists include albuterol (Proventil HFA, Ventolin HFA, ProAir), pirbuterol (Maxair), levalbuterol (Xopenex HFA) and alupent. These are taken “as needed” for quick relief of asthma symptoms and may be used before exercise to prevent exercise induced symptoms.
- Anticholinergics ( e.g., Atrovent=ipratropium bromide): Used to open the airways and are many times used with beta agonist to improve bronchodilation. May also be helpful when cough is prominent symptom.
Long-term, Controller Medications:
Anti-inflammatory Drugs: control inflammation of the bronchial tubes. Prevent asthma symptoms by reducing the ever- present inflammation of the airway lining. They take time to work, and must be used on a regular basis. There are three families of anti inflammatory drugs.
- Steroids: Inhaled steroids are “cortisone like” steroids which work locally in the lungs to decrease inflammation. (e.g., Asmanex, Azmacort, Vanceril, QVAR, Aerobid, Flovent, Pulmicort). Systemic steroids (e.g. prednisone, Medrol) are strong inflammatory drugs most often used in short courses (about 3-7 days).
- Leukotriene blockers: Medications which block the receptors for leukotrienes (Accolate, Singulair) or block the synthesis of leukotriense (Zyflo ). Leukotrienes are cellular mediators which lead to bronchial inflammation and narrowing, and cause an increase in mucus production in the bronchial tubes.
- Combination Inhaled steroid/ Long-acting Bronchodilator (e.g. Advair Diskus, Advair HF A, Symbicort)
- Cromolyn (Intal) and nedocromil (Tilade)
Bronchodialators:
- Long-acting bronchodilators ( e.g. Serevent, Foradil) Should not be used as “rescue” medication or alone as controller.
- Theophylline (e.g. , Theo-24, Uniphyl ): oral bronchodilator to be taken on a regular, longterm basis.
Potential Side effects
- Bronchodilators: increased heart rate, jitteriness
- Inhaled steroids: thrush, hoarseness
- Long-acting bronchodilators: potential increased risk of rare, serious life threatening asthma attacks
- Oral steroids (short term use) increased appetite, weight gain, water retention, moodiness, irritability, insomnia, stomach upset
- Oral steroids (long term use), growth suppression, cataracts, glaucoma, osteopenia/osteoporosis
What Happens During An Asthma
Flare-Up?
Asthma symptoms occur when there is blockage of the bronchial tubes, causing a whistling noise called “wheezing”, cough, shortness of breath, and/or chest tightness. This blockage is caused by three things:
- Swelling or “edema”: the lining of the bronchial tubes swells, expanding inward, making the size of the airway smaller. This swelling is caused by increased inflammation of the bronchial tube lining.
- Mucus secretion: the tissues that line the bronchial tubes secrete extra mucus which can plug the narrowed air passages even further.
- Bronchospasm: the muscles that surround the bronchial tubes tighten and make the airway even smaller.
Together, the swelling, mucus, and bronchospasm in the airways make it harder to move air through the bronchial tubes. The person with asthma must work harder and breathe faster to move air through these narrowed airways.
How Can I Prevent Asthma Symptoms From Becoming More Severe?
- A void the asthma triggers that may be causing the symptoms.
- Learn to recognize early warning signs
- Stop what you are doing, rest, and take slow deep breaths.
- Sip warm fluids to help relax
- Take two puffs of your bronchodilator inhaler to help relieve your symptoms
- Follow your asthma management plan
When Do I Call the Doctor’s Office?
Sometimes asthma episodes become more severe despite your best efforts to treat them early. A change or increase in medications or further medical treatment may be needed. Call your doctor’s office or seek medical help if:
- Asthma symptoms continue or worsen despite all treatment steps that your physician has given you
- The medicines are not helping or not lasting as long as they should.
- You have any doubt about the severity of an attack